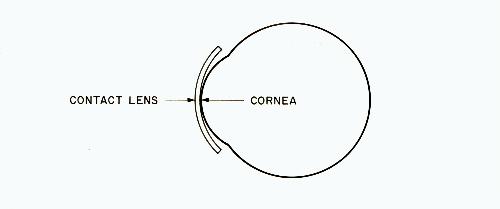
Fig. 1
Chapter 13
CONTACT LENSES AND ORTHOKERATOLOCY
Contact lenses are extremely thin wafers of plastic which are worn directly on the cornea. They actually rest on the film of tears located between the contact lens and the cornea.
The original contact lenses were made of hard plastic and many of the lenses sold today are still of this type. In recent years, contact lenses made of soft plastic material have also become popular. have made them more affordable and accessible.
First of all, don't be fooled by claims that wearing contact lenses instead of glasses will result in halting or slowing the progression of myopia. It is not possible to relax a ciliary spasm or prevent the elongation of the eye by merely wearing minus contacts instead of minus glasses. Many doctors make this claim. Some of them do it because more profit can be made selling contacts than in selling glasses. Others may genuinely believe what they say, but there is no concrete evidence to support the belief that minus contacts on myopes are significantly less harmful than minus glasses.
Many people turn from glasses to contacts in their late teens and early twenties, at the age when their myopia progression would have slowed or halted anyway. They can be easily misled into believing that the contacts had a beneficial effect. Then too, hard contact lenses frequently cause a change in the shape of the cornea that results in improved visual acuity when the lenses are removed. It is easy to believe that the course of the myopia has been reversed by the contacts. However, unless the contacts are worn regularly, the cornea will probably return to its original shape.
Keeping in mind then that the use of contact lenses is not a method of myopia prevention, let us examine a special use of contacts that could be of interest to someone who is already nearsighted. This contact lens field is called orthokeratology (sometimes abbreviated as "ortho-K")
The field of orthokeratology had its beginnings around 1962 when the above-mentioned ability of contact lenses to change the refractive status of the eye began to be discussed in earnest.
The formal definition of orthokeratology is "the reduction or elimination of refractive anomalies and binocular dysfunctions by the programmed application of contact lenses." In simple terms, this means using contact lenses to change the shape of the cornea of the eye, and it is especially applicable to myopic eyes.
The majority of people who undergo orthokeratology are myopes. Very few are hyperopes. There are also a substantial number of people who use the method to treat astigmatism.
Orthokeratology developed more or less by accident. A number of years ago, optometrists began noticing that after certain of their patients had been wearing contacts for several months the curvature of their corneas had changed slightly. The curvature of the cornea can be measured very accurately with special instruments. Realizing that the vision of a myopic person could be improved if the cornea could be permanently flattened, they began to fit contacts in a manner which they hoped would bring about the greatest amount of flattening. Then when the maximum flattening had been obtained, they would change the contacts to try to bring about further flattening. Their efforts were successful. They reasoned that since corneal changes are inevitable when contact lenses are worn, why not try to make these changes occur in a useful manner, rather than haphazardly?
There are various approaches to the selection of the proper contacts to get these results, so only a very simplified explanation will be given here.
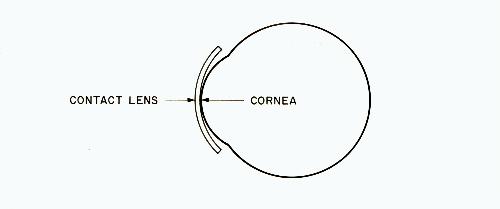
Fig. 1
Figure 1 shows an eye with a contact lens. Note that the contact lens is flatter than the cornea. The difference in curvature is greatly exaggerated for clarity.
It is easy to visualize from this diagram that if the cornea conforms to the contact over a period of time it will have become flatter. Then with the contact removed, the rays of light entering the eye will be bent less at the cornea than they were before the cornea was changed. These rays of light will thus come to a focus farther back in the eye, making the eye less myopic. Naturally, hard contacts, rather than soft contacts, have to be used since soft contacts would conform to the cornea - the opposite of what is intended.
Not all ortho-K lenses are fit flatter than the cornea. Many doctors claim that they give the patient the best fitting lens possible and they still get the desired alteration of the cornea.
Some ortho-K specialists say that the cornea is not "flattened" by this procedure - it is "made more spherical." Actually, both terms are accurate. The normal cornea is not a perfect sphere, but is shaped more like an ellipse. As the cornea is altered by the presence of the contact lens, the central portion of the cornea becomes flatter as the entire cornea becomes more spherical. Don't be misled into thinking that if your cornea is made more spherical it is being made more "normal." There is nothing wrong with the expression "flattening the cornea", and I believe that its use makes it easier for the public to visualize the way that ortho-K improves myopic vision.
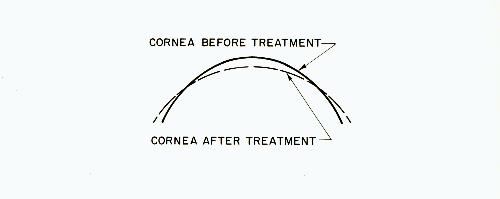
Fig. 2
In figure 2 the solid line shows the original corneal curve before treatment; the broken line shows how the shape of the cornea is changed by orthokeratology.
The average cornea has a radius of curvature of about 7.8 millimeters. The refractive power corresponding to this is about +43 D. If the radius of curvature of the cornea can be changed by only 0.5 millimeters its dioptic power will change by 3 D. Therefore, in the myopic eye, a 0.5-millimeter increase in the radius of curvature (flattening the cornea) will result in the elimination of 3 D of myopia.
After the cornea has been flattened a sufficient amount (a process that can take months or even years, depending on the initial amount of myopia), clear unaided vision is achieved.
In the usual treatment, the eyes are examined every six weeks or so, and as the cornea changes a different set of lenses is prescribed. The patient may receive five or six pairs the first year, three or four the second year, and two or three the third year. The cost for the complete treatment may be several thousand dollars. There are other drawbacks to orthokeratology in addition to its expense: it does not eliminate the cause of the myopia, and the results are usually not permanent.
This means that after clear unaided vision is attained, it is usualIy necessary to wear retainer lenses for part of the day. These are lenses that help retain the improvement that has occurred, to prevent the cornea from drifting hack toward its original shape. They are essentially the same as the lenses which the patient has been wearing for the treatment. They are just worn less often.
Some people have been able to retain their improvement by wearing the retaining contacts only when sleeping so that they are entirely free of the need for contacts or glasses during the day. There are some doctors who might not recommend such "night retainers" because they do not want to run the risk of injuring the eyes. Therefore you should certainly check with a vision specialist before wearing contacts while sleeping.
If retainers are not used, it is likely that in most cases the corneal curvature will slowly return to its original state.
It is logical to ask the question, "Why go to all that trouble and expense to improve the vision if you still have to wear retainers?" Many patients ask for orthokeratology in order to be accepted into a school, military position, or occupation that has vision requirements. Others simply have a desire to enhance their ability to see without the need of optical aids and the desire to be less dependent on external devices for normal vision. The occasional need for retainer lenses is acceptable to these people if it enables them to do many of the things that are restricted by the wearing of glasses or contacts.
Orthokeratology has been shown to be effective. In one two-year study involving 100 completed cases with an average beginning myopia of 2.5 D, the following results were obtained:1
| Amount of Beginning Myopia | No. of Patients Who Attained Emmetropia (No Myopia) |
|---|---|
| 0-2 D | 73% |
| 2-4 D | 36% |
| over 4 D | 22% |
Age seemed to have no effect on the results. The age of the patients varied from ten to fifty-two years.
The techniques of the various ortho-K specialists vary widely as do the results they obtain. The method is changing as new knowledge and experience are gained.
The amount that the cornea can be forced to change its shape is of course limited. One researcher gives the following practical limits to the amount of error that can reasonably be expected to be eliminated.1
Orthokeratology should not be used in beginning myopia when the myopia is caused only by a ciliary spasm. Instead, spastic myopia should be eliminated as quickly as possible by the teaching of proper close-work habits and by the use of preventive aids to inhibit the accommodation for close work.
If the cause of the acquired myopia is ignored, flattening of the cornea could be nearly as detrimental as the prescription of concave lenses, since both actions, by decreasing the convergence of the light rays entering the lens of the eye, make it necessary for the lens to accommodate more when focusing on an object at any given distance. This increased accommodation could aggravate the ciliary spasm and result in a further elongation of the eye, which will make necessary a further flattening of the cornea by continued orthokeratology treatment - the same vicious circle that concave lenses create. In adults, when the myopia progression has ceased, the above statement may not apply, hut it does apply to children. What is the sense of flattening the cornea to move the point of focus further back in the eye while we permit the eye to continue lengthening because of excessive close work?
The word orthokeratology comes from ortho, meaning correct or proper, and keratology, meaning having to do with the cornea. It thus means forming the cornea to a correct shape. This is certainly an accurate definition of what happens when a highly astigmatic cornea is made less astigmatic, but in the treatment of myopia it is somewhat of a misnomer. Most myopes have normal corneas. Orthokeratology is actually used to produce an abnormally shaped cornea to compensate for the abnormally long eye which has been produced by an abnormal amount of close work. It is difficult to suppress the thought that this is going about things in an abnormal way.
The importance of myopia prevention in conjunction with any orthokeratology program is recognized by some practitioners, but most ignore prevention. They reason that there is more money to be made in letting myopia develop and then trying to 'cure" it by orthokeratology. The entire medical business is built on such a foundation.
True myopia prevention means catching children before they become myopic. When the vision of schoolchildren is tested by unskilled people using nothing more than a wall chart, only those children who have already started to become myopic will be caught. The children who are just on the verge of moving into myopia or those who are rapidly approaching myopia are not caught. This is unfortunate because it is before myopia develops that preventive measures should be started. Proper vision examination methods should be used to see how much of a farsighted "cushion" each child has and whether or not this cushion is rapidly disappearing.
Orthokeratology has been compared to orthodontics (the straightening of crooked or cramped teeth by dentists), since both fields are concerned with correcting a physical defect. This is accurate as far as it goes, but there is an unspoken fallacy to this and many other aspects of health care. Let's take dentistry as an example.
Progressive researchers have known for many decades that most tooth decay and most birth defects result from faulty living. One of the best books on this subject was "Nutrition and Physical Degeneration", written by Weston Price, a dentist.2 Price traveled to many parts of the world and noted that as primitive societies began to get the food products of the more advanced societies (sugar, white flour, canned goods, etc.), tooth decay, birth defects and other health probIems increased rapidly, where they had been nearly unknown previously. Included in these problems was a poorly developed dental arch with insufficient room for the teeth to come in. Books like this should be required in every dental and medical school, but they are not. The public is told nothing about how to prevent their miseries because there is more money to be made in trying to cure them.
It is said by those who don't know any better that we don't need so many teeth for our modern life and our jaws are therefore getting smaller. The real reason is that the faulty diet of the mother, and later that of the child, results in faulty skeletal development, leaving insufficient room for the teeth. Since few people are interested in really improving the diet of the public, these myths are allowed to persist.
Orthodontics to correct cramped teeth and orthokeratology to correct myopia are thus involved with correcting something which could have been prevented.
Remember that orthokeratology is not a cure-all. It is not a form of myopia prevention, but is a technique which can be used when myopia has not been prevented, and irreversible axial-length myopia has occurred. There will be those who will lead the public to believe that myopia prevention and orthokeratology are synonymous. They are not. Myopia is an overelongation of the eye. Orthokeratology does nothing to alter or prevent this. Prevention is clearly better than cure.
Some orthokeratology specialists have even gone so far as to say that myopia is caused by a misshapen cornea and that by using orthokeratology they will press the cornea back to its proper shape. Those who make such erroneous claims are doing harm to the entire field of orthokeratology.
There are now hundreds of optometrists in the United States engaged in ortho-K work. They have treated many thousands of patients, and there is no evidence as yet that the process is in any way dangerous. However, very few ophthalmologists are using the procedure.